Vernooij LM, van Klei WA, Moons KG, Takada T, van Waes J, Damen JAAG. The comparative and added prognostic value of biomarkers to the Revised Cardiac Risk Index for preoperative prediction of major adverse cardiac events and all‐cause mortality in patients who undergo noncardiac surgery. Cochrane Database of Systematic Reviews 2021, Issue 12. Art. No.: CD013139. DOI: 10.1002/14651858.CD013139.pub2.
Picture this…
Haven is 47 years old, her health practitioner has recommended knee replacement surgery to help relieve the severe joint pain that she has been experiencing. Haven is anxious because she has heard mixed stories from friends about the risk of complications following surgery. Having researched the potential for complications online, Haven is aware that some people have particularly severe complications following surgery including heart-related complications that can lead to death. Haven’s health practitioner is reassuring and suggests that her risk of heart-related complications is low based on the Revised Cardiac Risk Index (RCRI). Using the RCRI the practitioner tries to estimate the likelihood of such a complication by taking into account Haven’s history of heart health, factors relating to other conditions such as diabetes mellitus or kidney problems, and whether or not her planned surgery is high risk. Though somewhat reassured, Haven wonders how accurate the prediction really is. She’d like to know if there are any other tools that could help make the prediction more accurate to help her to decide whether to go ahead.

Image 1: An image showing an operating theatre, showing a visual representation of the surgery discussed in the blog.
Photo by Endobariatric Endohospital on Unsplash
Summary messages –
- Using additional information, such as the presence of certain chemicals in the blood, to support the RCRI may make more accurate predictions about the chance of experiencing heart-related complications following surgery that is not heart-related.
- Risk assessment tools, other than the RCRI, might be better at predicting some complications following non-heart-related surgery, but not complications that are heart-related.
- Because of concerns about how the experiments that provided the information about accuracy were conducted, it is not possible to be 100% confident in these results.
What the research says –
- Why was research needed?
More and more people are receiving surgical treatment to improve their health and wellbeing or address health problems. Every operation has some risk of complications. Heart-related issues are responsible for less than 1 in 5 experiences of complications, but are the most likely to result in death. The ability to predict, in advance of an operation, which patients are at greatest risk of experiencing a heart-related complication, would help the health team to plan care and support that is most suited to the individual needs of the patient. Tools that are currently used to make these predictions can be inaccurate. This study was designed to bring together evidence about whether the current tool could be improved by taking into account additional information about the patient, or whether different tools could provide more accurate predictions on their own.
Additional information could be gather from so-called biomarkers, which are measurable signs that tell us how the body is doing. Examples of biomarkers include: measurements from blood, imaging techniques, age, smoking status and physical condition.
- What did they do?
The researchers sought the results of experiments that were conducted to answer one or more of the following questions in relation to predicting heart-related complications following surgery that is not heart-related:
- Does the addition of biomarkers increase the accuracy of the current tool?
- Can biomarkers make more accurate predictions on their own, than the current predictive tool?
- Are there other tools that are more accurate than the current tool?
Lots of experiments provided lots of different results for each of the questions. The researchers hoped to combine the results from all of the different studies on each topic to provide a single answer to each question. After making sure that the experiments contained useful information to answer one or more of the questions, a total of 107 experiments were identified. They were conducted by a wide range of researchers and involved patients who had received various types of non-heart-related surgery. The measures used to represent heart-related complications were not consistent in all studies making it difficult to combine results. Because the experiments were conducted in so many different ways, it was not possible for the researchers to combine the results. Instead, they had to look at each experiment individually to obtain a rough answer to the research questions.
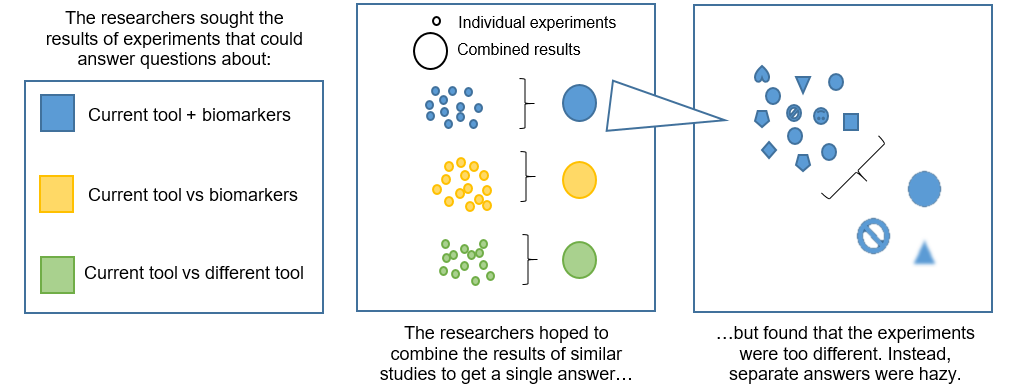
Image 2: A summary diagram showing the process to find and use results from the experiments.
Created by blog author Emily Taylor.
- What did they find?
Some biomarkers found in blood called brain natriuretic peptide or BNP for short and (NT-pro) brain natriuretic peptide (NT-proBNP) may improve the ability of the RCRI to predict heart-related complications following non-heart-related surgery. Two risk score tools seem to be better at predicting some complications following non-heart-related surgery, but not heart-related complications. However, because many of the experiments were found to have flaws in the way that they were carried out, researchers are not sure how much they can trust these results.
- What will this mean for patients?
For Haven, this means that, if her health practitioner was to recalculate her risk of heart-related complications using information about her blood biomarkers as well as the RCRI, the result could provide a more accurate prediction of a heart-related complication happening for her. If Haven wanted to know about her risk of complications that were not heart-related, then another risk tool might provide a more accurate prediction than the tool her health practitioner has already used (the RCRI). However, it is not possible to say for sure that this will be the case.

Image 3: An image showing a male doctor taking the blood pressure of a female patient. This illustrates the monitoring of certain cardiac symptoms. Photo by CDC on Unsplash
To be more confident that additions or alternatives to the current tool can really provide more accurate predictions, Haven would need to wait for more experiments to be conducted. The additional experiments would need to be conducted in a similar way, use similar measures to represent heart-related complications, be clear about the patients involved, and use similar methods to arrive at results.
Where is Haven now…
Haven was in a lot of pain from her knee and so made a decision to go ahead with the operation as planned. She knew that there was a possibility that the risk of her experiencing a heart-related complication could be higher or lower than what was calculated by the current risk tool, but decided that it was worth taking the risk in order to reduce her pain. When she recovered from her operation, Haven encouraged friends and relatives who were going for surgery that was not heart-related to take part in research if it was offered to them. That way she hoped that future patients would be able to have more confidence in their risk and be able to make decisions based on more accurate information.
Emily Taylor
PhD Student, College of Medicine and Health, University of Exeter (UK)
Please note: The stories and pictures used do not represent specific individuals – they are merely used to contextualise the data into a more digestible format.
Reference points –
Vernooij LM, van Klei WA, Moons KG, Takada T, van Waes J, Damen JAAG. The comparative and added prognostic value of biomarkers to the Revised Cardiac Risk Index for preoperative prediction of major adverse cardiac events and all‐cause mortality in patients who undergo noncardiac surgery. Cochrane Database of Systematic Reviews 2021, Issue 12. Art. No.: CD013139. DOI: 10.1002/14651858.CD013139.pub2.
Guidance sourced from https://uk.cochrane.org/choosing-images-sharing-evidence-guide
If you have any comments regarding this blog post, please contact us at globalageing@cochrane.org. We would love to hear your thoughts and answer any questions you may have.
Web editor: Monserrat Conde
